Serotonin (5-hydroxytryptamine, or 5-HT) is a powerful neurotransmitter with far-reaching effects on both mental and physical health. While often associated with mood regulation, its function is deeply integrated into various biological systems, including digestion, cognition, immunity, and circadian rhythm. Understanding the complex dynamics of serotonin—including how it’s influenced by genetics, medication, nutrition, and cellular biochemistry—can shed light on mental health conditions and overall well-being.
How Antidepressants Affect Serotonin
Selective Serotonin Reuptake Inhibitors (SSRIs) are the most common antidepressants. They work by blocking the reabsorption (reuptake) of serotonin into the presynaptic neuron, leaving more serotonin available in the synaptic cleft to stimulate the postsynaptic neuron.
Other antidepressants include:
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) – Target both serotonin and norepinephrine.
- MAOIs (Monoamine Oxidase Inhibitors) – Prevent breakdown of serotonin by inhibiting the enzyme monoamine oxidase.
- Tricyclics – Block reuptake of serotonin and norepinephrine but with more side effects.
Natural supplements can also influence serotonin:
- St. John's Wort – A plant extract with antidepressant effects, believed to inhibit the reuptake of serotonin, dopamine, and norepinephrine. It may enhance mood but also interacts with many medications, including SSRIs, and can increase the risk of serotonin syndrome.
- Saffron – Derived from Crocus sativus, saffron has shown promise in boosting serotonin levels and alleviating mild-to-moderate depression. Its active components, like crocin and safranal, are believed to modulate neurotransmitter activity and act as natural serotonin enhancers.
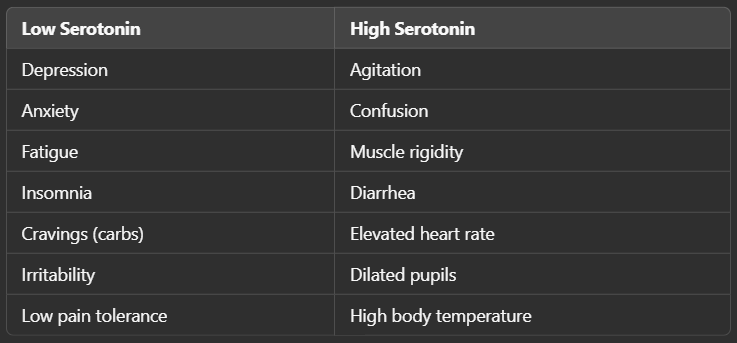
Symptoms of Low vs. High Serotonin Levels
Serotonin Syndrome: A Dangerous Excess
Serotonin syndrome is a potentially life-threatening condition caused by excess serotonin, often due to drug interactions or overdose (e.g., combining SSRIs with MAOIs or certain supplements like St. John's Wort).
Symptoms include:
- Mental status changes (confusion, hallucinations)
- Autonomic instability (fever, sweating, fast heart rate)
- Neuromuscular abnormalities (tremor, hyperreflexia, clonus)
- Gastrointestinal issues (nausea, diarrhea)
Emergency treatment involves stopping the offending agent and using serotonin antagonists like cyproheptadine if needed.
How to Distinguish Between High and Low Serotonin
Distinguishing isn't always straightforward, as symptoms can overlap with other conditions. Assessment includes:
- Symptom profiling
- Blood or urine serotonin levels (though not always accurate for brain levels)
- Genetic testing for SNPs in serotonin pathways
- Response to treatment (e.g., worsened symptoms on SSRIs may indicate high serotonin)
Genetic Factors Affecting Serotonin
Several genes influence serotonin synthesis, transport, metabolism, and receptor activity:
- TPH1/TPH2 – Tryptophan hydroxylase enzymes responsible for converting tryptophan to 5-HTP.
- SNPs here can slow production of serotonin from tryptophan.
- SNPs here can slow production of serotonin from tryptophan.
- SLC6A4 – Serotonin transporter gene (coding for the SERT protein).
- The famous 5-HTTLPR polymorphism affects reuptake speed—short variants are linked to anxiety and depression.
- The famous 5-HTTLPR polymorphism affects reuptake speed—short variants are linked to anxiety and depression.
- MAO-A – Monoamine oxidase enzyme that degrades serotonin.
- Fast variants clear serotonin quickly, possibly reducing brain levels.
- Fast variants clear serotonin quickly, possibly reducing brain levels.
- COMT – Though primarily involved in dopamine metabolism, it can indirectly affect serotonin pathways via methylation.
The Role of Receptors
There are 14+ serotonin receptor subtypes (e.g., 5-HT1A, 5-HT2A, 5-HT3). Their distribution and function vary:
- 5-HT1A (HTR1A gene) – Found both presynaptically and postsynaptically. As a presynaptic autoreceptor, it inhibits further serotonin release when activated, acting as a regulatory brake. Postsynaptically, it plays a crucial role in mood regulation and anxiety. Variants in the HTR1A gene have been linked to increased risk of depression and altered antidepressant response. Downregulation of HTR1A may lead to increased serotonergic activity, while upregulation could blunt the release of serotonin.
- 5-HT2A (HTR2A gene) – Located primarily postsynaptically, this receptor modulates perception, cognition, and mood. Activation can enhance excitatory neurotransmission. It's also the target of many psychedelics (e.g., LSD, psilocybin). Certain polymorphisms in the HTR2A gene can influence how individuals respond to SSRIs and are associated with psychiatric conditions like schizophrenia and major depressive disorder. In bipolar disorder, upregulation of HTR2A has been observed in manic phases, potentially contributing to heightened excitability, while downregulation may relate to depressive symptoms.
- 5-HT3 – Found in the gut; targeted by anti-nausea drugs.
Genetic polymorphisms in these receptors can alter sensitivity, meaning even normal serotonin levels may not function properly. Dysregulation of HTR genes has been implicated in various mental health disorders:
- Bipolar disorder – Altered expression of HTR1A and HTR2A may influence phase cycling and treatment responsiveness.
- Major depressive disorder – Reduced HTR1A binding is often found, particularly in treatment-resistant cases.
- Anxiety disorders – Variants that reduce HTR1A activity may increase vulnerability to chronic anxiety.
- Schizophrenia – HTR2A dysfunction is linked to altered sensory processing and hallucinations.
Cofactors and Inhibitors (Nutrition Link)
Several nutrients act as cofactors for serotonin synthesis and metabolism:

Inhibitors include:
- Cortisol – High stress can lower serotonin synthesis.
- Inflammation – Cytokines can divert tryptophan away from serotonin.
Quinolinic Acid, NAD+, and the Kynurenine Pathway
When inflammation is high, tryptophan is diverted away from serotonin and into the kynurenine pathway, producing:
- Quinolinic acid – Neurotoxic, associated with depression and neurodegeneration.
- Kynurenic acid – Neuroprotective (in balance).
- NAD+ – A critical coenzyme for mitochondrial function and cellular energy.
This diversion can lower serotonin availability and increase neurotoxic load. This explains why chronic inflammation is often linked to depression.
SNPs: Fast vs. Slow Variants
Single Nucleotide Polymorphisms (SNPs) can affect enzyme speed:
- Fast metabolizers (e.g., MAO-A) may degrade serotonin too quickly → low brain levels.
- Slow metabolizers might have high serotonin at the synapse, increasing risk of serotonin syndrome or overstimulation symptoms.
Personalized medicine, including genetic testing, helps tailor treatment (e.g., choosing the right antidepressant or dosing strategy).
Creativity and Serotonin
Serotonin may also influence creativity, particularly through its interaction with the 5-HT2A receptor. Activation of 5-HT2A has been linked to enhanced cognitive flexibility, abstract thinking, and associative learning—all of which are key components of creative thought. This receptor is also targeted by psychedelic compounds, which are known to temporarily alter perception and thought patterns, often increasing divergent thinking and openness to experience.
Studies suggest that individuals with certain HTR2A polymorphisms may have increased sensitivity to stimuli and unconventional thinking styles, traits commonly associated with creativity. Moreover, balanced serotonergic function appears important for maintaining the cognitive stability-flexibility balance, which supports both goal-directed behavior and spontaneous insight generation.
Summary
Serotonin is a complex, vital neurotransmitter with widespread influence. Its balance is determined by many factors:
- Medications and receptor activity
- Genetic variants in synthesis, transport, and breakdown
- Nutrition, including cofactors and inflammatory status
- Biochemical pathways like kynurenine and NAD+ production
- Regulation of HTR genes and receptor sensitivity
Understanding these dynamics can guide personalized approaches to treating mood disorders, gut issues, and even neurodegenerative diseases.

